Comparing Colonoscopy Screening to Other Cancer Tests
When it comes to early detection of cancer, regular screenings are one of the most effective tools available. Among these, colonoscopy screening is considered the gold standard for detecting colorectal cancer, especially in individuals over the age of 50 or those with a family history.
However, other types of cancer screenings—such as mammograms, Pap smears, PSA tests, and low-dose CT scans—are also used to identify cancer in its early stages. Understanding how colon screening tests work compared to other tests helps patients and caregivers make informed decisions about preventive care.
What Is Colonoscopy Screening?
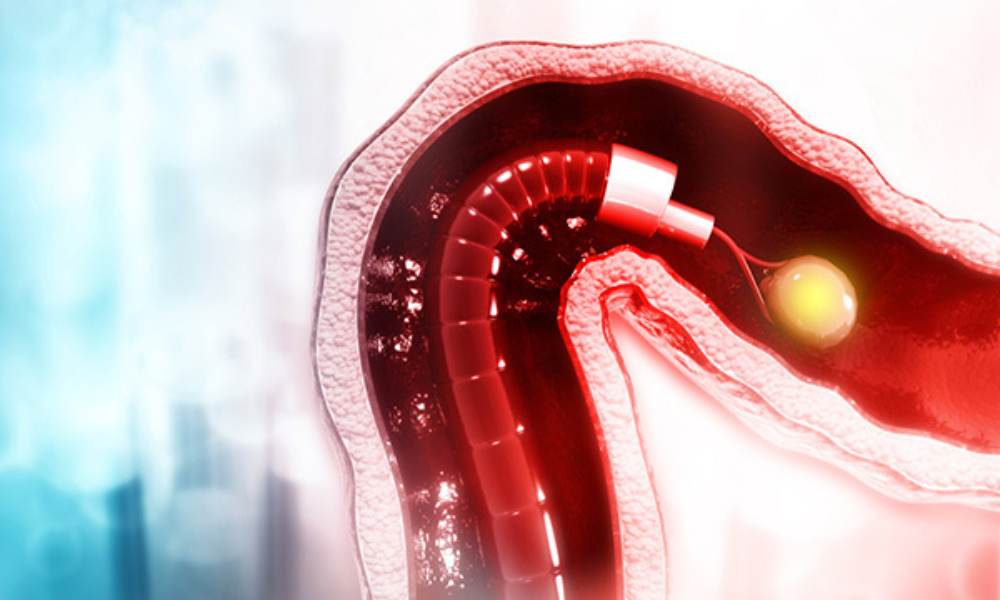
Colon cancer screening involves the insertion of a long, flexible tube with a camera into the rectum to examine the colon and rectum for abnormalities such as polyps, ulcers, or tumors. It is both diagnostic and preventive, as doctors can remove pre-cancerous polyps during the same procedure, reducing the risk of developing colorectal cancer.
This type of screening is typically recommended starting at age 50, though it may be advised earlier for individuals with increased risk factors, such as inflammatory bowel disease or a family history of colorectal cancer. Colonoscopy screening is usually repeated every 10 years if no issues are found, making it a comprehensive but less frequent method compared to some other cancer tests.
Colonoscopy vs. Fecal-Based Tests for Colon Cancer
While colonoscopy is the most thorough method for colon cancer detection, other tests like the Fecal Immunochemical Test (FIT) and guaiac-based fecal occult blood test (gFOBT) offer non-invasive alternatives. These tests detect hidden blood in the stool, which can be a sign of colorectal cancer or large polyps.
They are less invasive and can be done at home, but they require more frequent testing—usually once a year—and lack the ability to remove polyps or visually examine the colon.
Another option, the stool DNA test (e.g., Cologuard), combines FIT with genetic markers linked to cancer. It’s more accurate than FIT alone but still not a replacement for the direct visual inspection that colonoscopy provides. If any of these tests return positive, a follow-up colonoscopy is usually required for confirmation and further action.
Comparing with Mammograms for Breast Cancer
Mammograms are X-ray images of the breast used to detect breast cancer early, often before any symptoms appear. While mammograms are recommended annually or biennially for women over 40 or 50 (depending on guidelines), they only screen for one type of cancer.
In contrast, colonoscopy screening targets colorectal cancer, which is the third most common cancer worldwide. Both screenings are vital and address different risk areas, but they follow similar principles—early detection leads to more successful treatment outcomes.
Mammograms are quicker and less invasive than colonoscopies, though they do involve exposure to low-dose radiation. Unlike colonoscopy, they cannot prevent cancer by removing pre-cancerous tissue.
Colonoscopy vs. Pap Smear and HPV Test for Cervical Cancer
Pap smears and HPV tests are used to detect cervical cancer or the presence of high-risk HPV strains. These tests are generally done during a pelvic exam and are recommended every three to five years for women aged 21 to 65. While these tests are highly effective in reducing cervical cancer rates, they apply only to the female population.
Colonoscopy screening, on the other hand, is recommended for all adults within a certain age range, regardless of gender. Both types of screening have been pivotal in reducing cancer mortality rates, and neither should be viewed as more important—rather, they serve complementary roles in a holistic preventive healthcare plan.
Comparing with PSA Testing for Prostate Cancer
Prostate-Specific Antigen (PSA) testing measures the level of PSA in a man’s blood and is commonly used to screen for prostate cancer. While less invasive than a colonoscopy, PSA testing has a higher rate of false positives, which can lead to unnecessary biopsies and anxiety.
Unlike colonoscopy, it doesn’t provide a direct look at the affected area or offer the ability to treat during screening.
Colonoscopy screening has a more defined protocol and fewer ambiguous results, making it a more definitive tool in its area of focus. However, PSA testing remains important for men over 50, particularly those with a family history of prostate cancer.
Screening for Lung Cancer
Low-dose CT scans are used to detect lung cancer in high-risk individuals, particularly long-term smokers. These scans can identify tumors before symptoms begin, but like PSA testing, they come with a risk of false positives and incidental findings that may lead to further testing.
Colonoscopy screening, by contrast, offers both diagnosis and immediate intervention, and carries a lower risk of such complications. Each test has its place depending on the patient’s history, age, and risk profile.
Conclusion
Colonoscopy screening stands out for its dual role in diagnosing and preventing colorectal cancer by removing polyps during the procedure. Compared to other cancer tests—such as mammograms, Pap smears, PSA tests, and low-dose CT scans—it is more invasive but offers unmatched value in colorectal cancer prevention. While no single test covers all cancer risks, incorporating colonoscopy screening alongside other routine cancer checks forms a strong foundation for early detection and improved long-term outcomes.











